FDA wants trials to include obese patients. Modeling will help
On November 9, FDA held a workshop to explore whether obese patients should be included in drug trials. This may translate into requirements for all drug studies to include obese individuals. If so, drug development costs and timelines would rocket, without support from tools like in silico trials and virtual populations. These are already breaking into the mainstream, and are likely to become more critical still to enabling accurate, efficient, R&D.
With close to half of the US adult population now obese or severely obese, this is no longer a ‘special population’. Childhood obesity has increased eightfold in the last 40 years, affecting more than 380 million children worldwide. That’s why understanding how drugs may behave differently in obese patients relative to normal-weight patients, and adjusting dosing and regimens accordingly, is not simply a reasonable quest. It’s an urgent one.
“The implications of obesity cannot be overstated,” declared FDA Commissioner Robert Califf at the start of the workshop. Yet there’s a “deficit of evidence about medicines in obese patients,” he continued. For now, FDA doesn’t require sponsors to include obese patients in trials. Yet several invited experts, including David Greenblatt, professor at Tufts University School of Medicine, called for mandatory study of obese patients in all new drug trials. FDA’s own blurb for the event declared that such patients “should be included in drug development studies.”
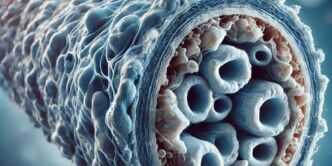
Obesity brings many physiological changes besides greater body mass. Cardiac output and liver blood flow increase, as does gut wall permeability and underlying inflammation, thanks to cytokines and hormones secreted by adipose tissue. Levels of some drug-metabolizing enzymes change.
Yet specific dosing guidelines for obese adults or children are missing, despite concrete evidence that some drugs have half-lives over five times longer in obese patients than normal weight individuals. Studies dating back several decades show that it can take longer for obese people to achieve effective drug concentrations and full wash-out. This has implications for the effectiveness of oral emergency contraceptive pills, among many other medications.
Obese patients often have co-morbidities such as diabetes, heart or liver disease. That’s one reason they aren’t adequately represented in many trials. Another is the stigma associated with the condition, which many still don’t recognise as a disease. Finally, socio-economic and ethnic disparities make this a complex area: black Hispanic women have the highest rates of obesity according to Frank Hu, Harvard Medical school, and the condition is also strongly correlated with education levels. FDA in April 2022 released draft guidance calling for greater racial and ethnic diversity in clinical trials, recommending that sponsors submit a diversity plan early in development.
If similar guidance is published in relation to obese patients, in silico modelling would provide an efficient, accurate tool to help industry progress toward more appropriate dosing in this group. Fittingly, modeling’s promise featured prominently at the workshop. Hao Zhu, FDA’s director of pharmacometrics in the Office of Pharmacology, pointed to its unique potential to generate evidence for dose-optimisation, by integrating all the variables impacted by body weight. “There are lots of examples where model-informed drug development approaches have been used to support a new dosing regimen not directly tested in trials,” he said.
There may soon be even more. FDA talks of innovative solutions to improve data generation and analysis. “We need approaches to clinical studies that allow incorporation of these tools at limited cost,” concluded Califf.